Copilot for Health Innovation
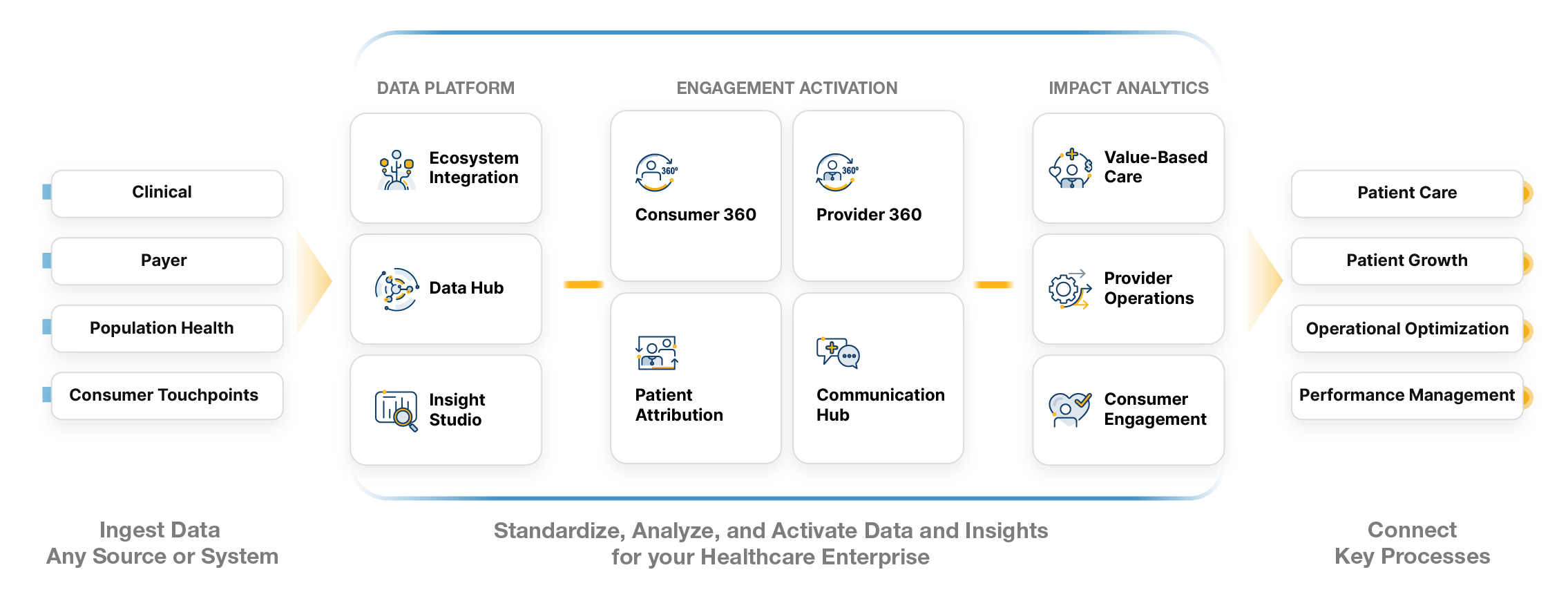
Unlock Value with Leap
Winning Solutions
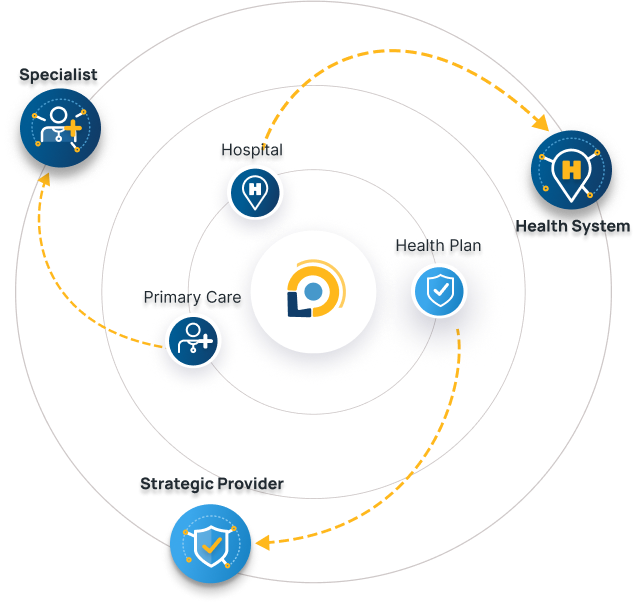
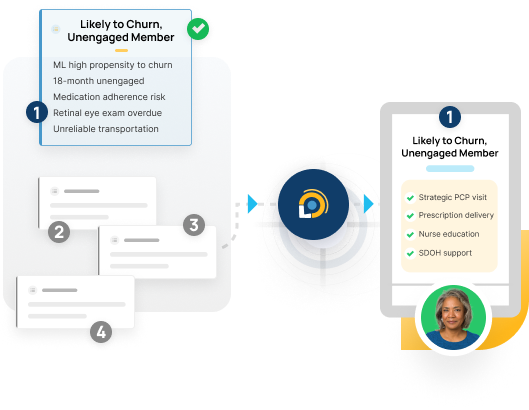
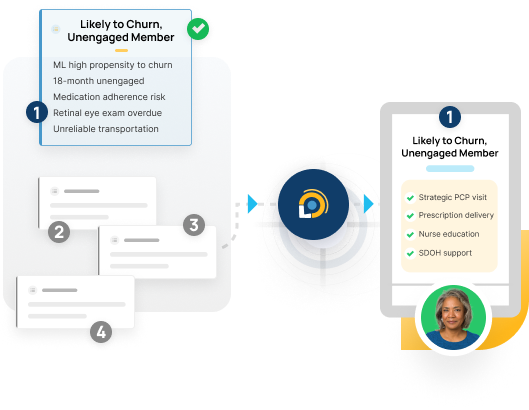
We meet you where you are, providing immediate value whether your focus is revenue growth, consumer engagement, experience improvement, provider operational efficiency, or value-based care performance. Our solutions drive better outcomes and better business.
Efficiently acquire and retain members with our insight-driven omnichannel campaign management service, seamlessly connected to your sales channels. Drive growth by leveraging our Leap platform and experienced database marketing team.
Results
We drive measurable value aligned to your priorities.
Increased Revenue
5:1+
Expected ROI
Acquire consumers, increase appointments and reduce ecosystem leakage
Optimize Clinical Resources
30+%
Resource Optimization Lift
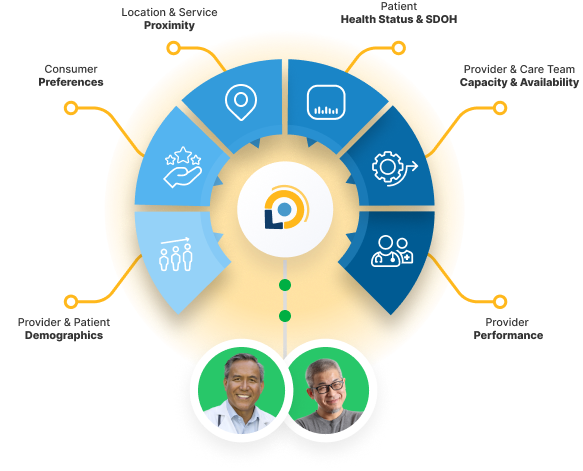
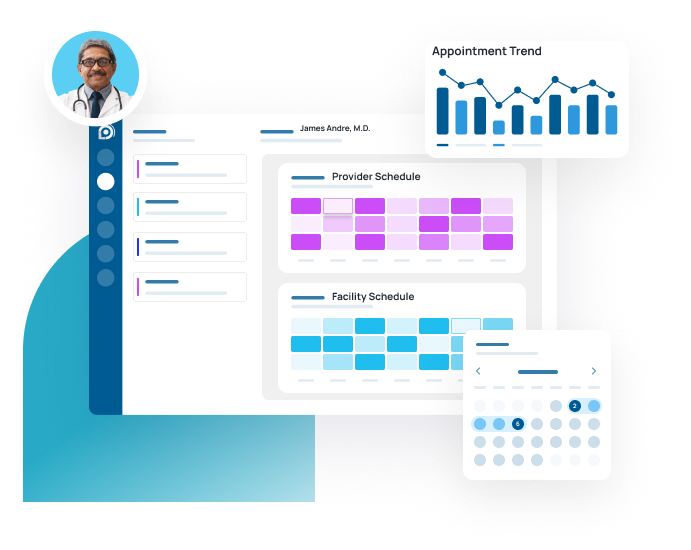
Reduce unused capacity, match patient to optimal providers and load-balance schedules
Improve Operational Efficiency
40+%
Reduce Administrative Expense
Optimize analyst time and engage consumers through your digital front door